I guess a lot of women talk about Menopause, why? Well, because every woman has to go through it, but not every woman will experience it in the same way. Let’s get some facts straight.
What is menopause?
Menopause is defined as the stage when a woman reaches the end of her reproductive cycle and stops menstruation (periods).
When?
The average age that menopause takes place is 51 years however, 1 in 100 women suffer from early menopause and therefore the average age may vary widely.
Why? Why only women?
Menopause is caused by a change in the balance of the body’s sex hormones, this happens naturally as you get older. It takes place when your ovaries stop producing as much of the hormone oestrogen and therefore will no longer release an egg each month. Premature or early menopause can occur at any age, and in many cases there’s no clear cause.
What happens when oestrogen levels are low?
Reduced oestrogen levels can have many effects on a woman’s body including irregular periods, hot flushes, mood changes, lack of sex drive and vaginal dryness. This can all contribute to a loss in quality of life1. Prolonged lack of oestrogen can also contribute to several long-term conditions including, osteoporosis2.
Symptom check list:
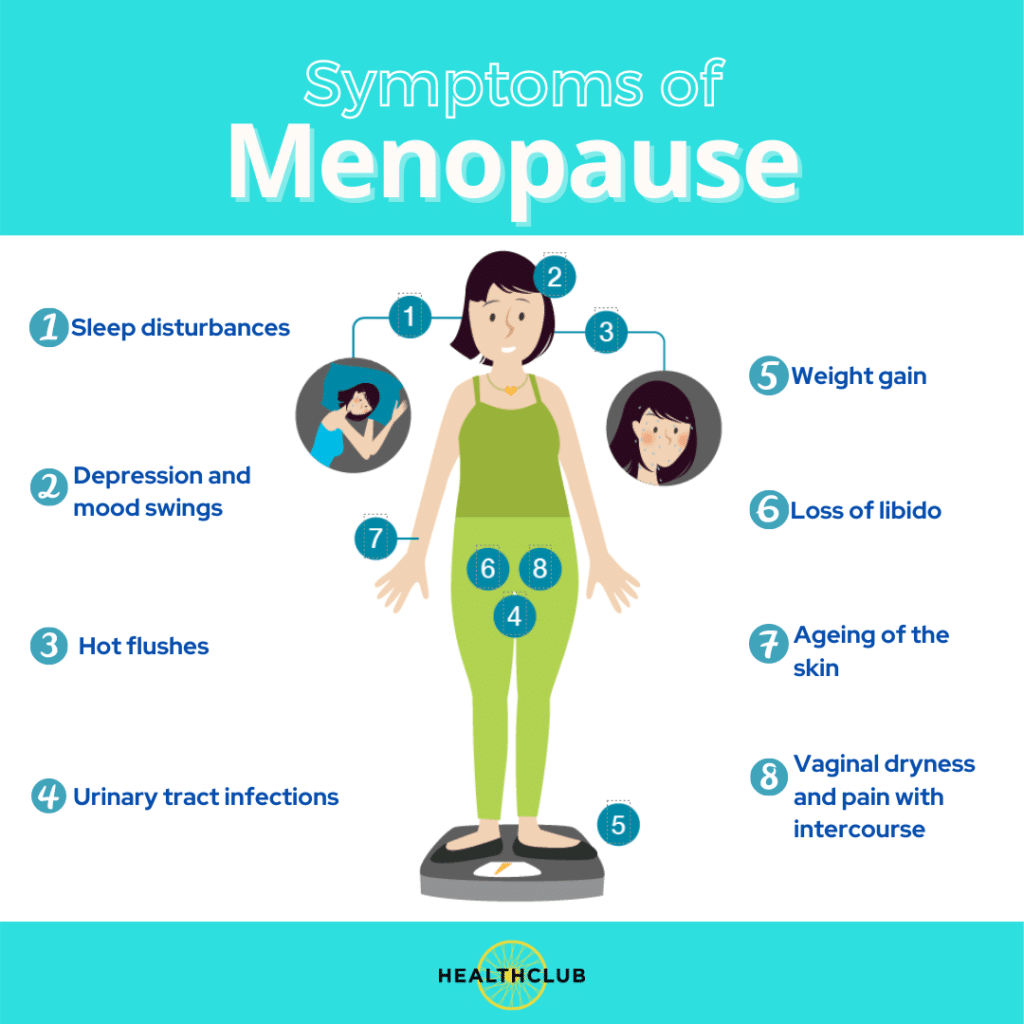
- Day time / night time sweats & flushes
- Unable to sleep
- Headaches
- Tiredness
- Loss of energy
- General aches & pains
- General itchiness
- Formication (feeling of something crawling over you)
- Changes in hair
- Emotional, tearful
- Depression
- Anxiety
- Panic attacks
- Palpitations
- Alteration in bladder function
- Vaginal dryness/soreness
- Vaginal itching
- Soreness / pain with intercourse
- Bleeding with intercourse
- Loss of libido (sex drive)
- Difficulty achieving orgasm
- Alteration in periods
The above symptoms are known as short term symptoms of the menopause.
Long term symptoms may include;
- Bone loss – osteoporosis
- Connective Tissue – Skin & Cartilages
- Cardiovascular – Myocardial Infarcts
- Cardiovascular accident/ stroke
- Alzheimer’s
So, what can be done?
Well firstly it is important to speak to your GP who, may offer advice or refer you to a gynecologist, it really depends on whether they feel confident on the subject and prescribing what is available on the market.
What is available to help women who are in The Menopause
There are several different types of treatments available; ones that directly replace the hormones and others which are targeted towards reducing specific symptoms.
Let’s talk Hormone Replacement Therapy – HRT
HRT Hormones
The 2 main hormones used in HRT are:
- oestrogen – types used include estradiol, estrone and estriol
- progestogen – a synthetic version of the hormone progesterone, such as dydrogesterone, medroxyprogesterone, norethisterone and levonorgestrel
HRT involves either taking both of these hormones (combined HRT) or just taking oestrogen (oestrogen-only HRT). Most women take combined HRT because taking oestrogen on its own can increase your risk of developing womb (endometrial) cancer. Taking progestogen alongside oestrogen reduces this risk. Women who do not have a womb due to a hysterectomy take oestrogen alone.
There are different ways of taking HRT, these include tablet from, skin patches, gels, vaginal creams, pessaries or rings.
How to get started on HRT
As mentioned above you must speak to your GP or gynecologist. Your healthcare provider will explain the types of HRT available. You’ll usually start with a low dose, which may be increased at a later stage, depending on whether your symptoms would have improved or not. However, it is important to keep in mind that it may take a few weeks to feel the effects of the treatment. It is recommended to give the treatment three months to work, if no improvements are reported the dose of the HRT may be increased, or type of HRT may be changed.
Who can take HRT
Most women can have HRT if their symptoms are associated with the menopause. But HRT may not be suitable if you;
- Have a history of breast cancer, ovarian cancer or womb cancer.
- Have a history of blood clots.
- Have untreated high blood pressure – this needs to be controlled before starting HRT.
- Have liver disease.
- Are pregnant. One can still get pregnant while taking HRT, therefore is it recommended to you contraception up to two years after your last period if you are under 50 years or for one year if over the age of 50.
In the above circumstances, alternatives to HRT may be recommended.
Alternative treatments
If you are unable to take HRT or decide not to, you may want to consider alternative ways of controlling your menopausal symptoms, these include.
- lifestyle changes such as exercising regularly, eating a healthy diet, cutting down on coffee, alcohol and spicy foods, and stopping smoking
- tibolone – a medicine that is similar to combined HRT (oestrogen and progestogen), but may not be as effective and is only suitable for women who had their last period more than 1 year ago
- antidepressants – some antidepressants can help with hot flushes and night sweats, although they can also cause unpleasant side effects such as agitation and dizziness
- clonidine – a non-hormonal medicine that may help reduce hot flushes and night sweats in some women, although any benefits are likely to be small
HRT treatment regimes
Treatment plans for HRT may vary, and therefore it is best to leave it up to your healthcare provider to identify which one would suit you best.
The 2 types of routines are cyclical (or sequential) HRT and continuous combined HRT.
- Sequential HRT
Sequential HRT is often recommended for women taking combined HRT who have menopausal symptoms but still see a period, also known as peri menopausal. With this type of HRT you take oestrogen every day, and take progestogen alongside it for the last 14 days of your menstrual cycle
- Continuous Combined HRT
Continuous combined HRT is usually recommended for women who are postmenopausal. A woman is usually said to be postmenopausal if she has not had a period for 1 year. This type of HRT involves taking oestrogen and progestogen every day without a break.
Oestrogen-only HRT is also usually taken every day without a break.
How long can you take HRT for?
There is really no limit, but it is important to speak to the healthcare professional who initially prescribed the treatment, they will give you an indication for how long you will need to take HRT or whether it would be the right time to stop it. Most women stop taking it once their menopausal symptoms pass, which is usually after a few years. When you decide to stop, you can choose to do so suddenly or gradually. Gradually decreasing your HRT dose is usually recommended because it’s less likely to cause your symptoms to come back in the short term. Contact a GP if you have symptoms that persist for several months after you stop HRT, or if you have particularly severe symptoms. You may need to start HRT again.
Side effects of HRT
It is good to keep in mind that side effects caused by HRT will usually pass within 3 months of starting treatment.
Common side effects include:
- breast tenderness
- headaches
- feeling sick
- indigestion
- abdominal (tummy) pain
- vaginal bleeding
What do we recommend?
Nowadays women in the menopause may often be overwhelmed with life in general. Going through the menopause may make situations worse. Therefore, we suggest if one is experiencing symptoms that are affecting their day to day living or mood it is recommended to seek the advice of their GP or gynecologist.
What are our conclusions?
‘HRT – a highly successful treatment for common symptoms of the menopause’2
HRT can help with common symptoms of the menopause such as hot flushes, sweats and low mood2
HRT treatments also have long term benefits for example the risk of fragility fracture while taking HRT is reduced. There were 23 fewer cases of fragility fracture amongst women taking HRT compared with no HRT or placebo2
Not all HRT treatments are the same – it is important to discuss the treatment options available with your GP, including the benefits and safety profiles of each, to ensure you receive a tailored treatment.
- British Menopause Society (BMS). Are women suffering in silence? May 2017.
- NICE full guidance on Menopause Diagnosis and Management. November 2015.




